Multiple sclerosis (MS) is a chronic disease, classified as an autoimmune disease that attacks the central nervous system (brain, spinal cord, and optic nerves). It affects approximately 2.4 million people and is more prevalent in women, with a ratio of women to men at 2:1. More Canadians are diagnosed with MS than in almost any other nation, with more than 77,000 cases active in this country.
MS can be unpredictable in when it appears and what symptoms it will present. The disease will disable some people quickly and others slowly. At times, people may not experience symptoms for years and then suddenly the disease can become active and the progression to disability can accelerate. Still others experience mild symptoms that don’t quickly progress.
What causes multiple sclerosis?
While the official stance is that the cause of MS is unknown, there is over 30 years of research that points to a different conclusion on what causes multiple sclerosis:
- collection of chronic infections
- infestation of parasites
- Lyme disease
- fungal overgrowth
- bacterial infections in the body
- high stress
- sleep deprivation
- subsequent use of antibiotics
- environmental toxins
- exposure to wireless radiation
- mould indoor
MS and chronic disease in general, is caused by a collection of chronic infections. Studies have shown the link between infections such as parasites, Lyme disease, and fungal overgrowth, offering compelling evidence for a causal link.
While the mainstream medical community concludes that we don’t know the direct cause of MS, ample peer reviewed scientific research shows that we do: multiple sclerosis is caused by an infestation of parasites, fungus and bacterial infections in the body. This invasion causes significant inflammation and immune dysfunction.
When the immune system is compromised by chronic infections, environmental factors such as (but not limited to) high stress, sleep deprivation, other infections, subsequent use of antibiotics, environmental toxins, and the exposure to wireless radiation and/or mould in the home or working environment all further weaken the immune system. In this state, the infections become more active – consequently triggering an MS attack.
Understanding this connection between infection (in the form of parasites, fungal overgrowth, and bacterial infection), combined with how well the immune system is functioning, is the basis to move forward and recover from MS.
MS inside the body
Electrical signals travel from the brain to the body and back via nerve highways. It takes about one-thousandth of a second for a neuron to fire an impulse and return to its resting level. A maximum of 1,000 nerve impulses per second is possible but the average is closer to 300-400 impulses per second.
Each nerve impulse sends another signal through the nerves in the body, and each nerve is protected and insulated by a fatty casing called a myelin sheath.
MS attacks this essential part of the nerve
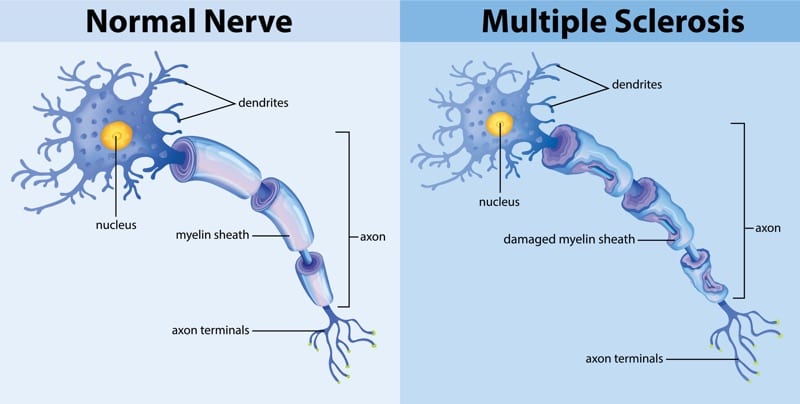
As the myelin becomes inflamed and eventually breaks down over time, scar tissue replaces it. As a result, the nerve cannot transmit the signal as effectively between the brain and the body, and thus there is lag or an inability for the nerve signal to reach its destination. This is when the symptoms of MS begin to appear.
What is an autoimmune disease?
Our standard of care believes that autoimmune disease is a condition in which the immune system mistakenly attacks the body, instead of protecting it.
For at least 30 years, medically trained doctors and researchers have understood that that autoimmune disease is caused by chronic silent infections in the body. Science has discovered that there are at least 17 ways that disease causing microbes (bacteria, fungi and parasites) can cause immune dysfunction and inflammation.
MS and Parasites

More and more research is linking the health of the gut microbiota — the ecosystem of bacteria that lives within the digestive tract — to an array of diseases that can occur throughout the body, including mental health issues. In terms of multiple sclerosis, studies are showing that when certain bacteria are absent from the body, MS is more active.
According to research and published in a study called The Gut Biome in Multiple Sclerosis , “the gut microbiome has been shown to have profound effects on the development and maintenance of immune system in both animal models and in humans. A growing body of evidence has implicated the human gut microbiome in a range of disorders, including obesity, inflammatory bowel diseases, and cardiovascular disease.”
The study further claims that “animal studies present compelling evidence that the gut microbiome plays a significant role in the progression of demyelinating disease, and that modulation of the microbiome can lead to either exacerbation or amelioration of symptoms.”
Evidence that people with MS have lower levels of good or healthy gut bacteria is so compelling that the National MS Society invested $28M into new research that investigates the link between gut wellness and the disease that affects so many.
MS and Fungal Overgrowth

Another causal link for people living with multiple sclerosis connects fungal overgrowth within the body to the root cause of the disease.
In a study titled Fungal toxins and multiple sclerosis: a compelling connection, researchers propose ”fungal toxins are the underlying cause of multiple sclerosis and thus may offer an avenue towards an effective cure.”
The body of research is large. Another paper called Multiple sclerosis and mixed microbial infections. Direct identification of fungi and bacteria in nervous tissue was published in 2016. It reports that there is a demonstration that certain bacteria are present in central nervous system tissue, and not in a control group, which points to a direct involvement of microbial infections in the causation of MS.
It goes on to claim that their “present observations point to the novel concept that MS could be caused by polymicrobial infections.”
MS and Lyme Disease

Lyme disease has gained more attention in the last few years, though reported cases remain fairly consistent.
But the link between Lyme disease and MS is becoming easier to find.
Dr. Stephen Phillips, past president of the International Lyme and Associated Diseases Society, has presented evidence at scientific conferences that there is an association between MS and Lyme disease. Even anecdotally, he treats an abnormally high number of MS patients in his practice.
The similarities in symptoms between the two diseases are interesting to see side by side. Dr. Patricia Coyle of SUNY- Stony Brook presented research on how to differentiate between MS and Lyme at a Lyme Disease Foundation conference. Her work showed that the similarities include the following:
- Both cause optic neuritis, inflammation of the optic nerve, and blindness.
- Both cause white spots or demyelinating lesions visible on an MRI scan of the brain.
- Both could cause paresthesia – tingling and numbness of the extremities.
- Both can cause bladder dysfunction.
- Both have relapsing, remitting nature.
- Both diseases can cause elevations of myelin basic protein (MBP) and oligoclonal bands (immunoglobulins) to appear in the spinal fluid.
However there are some differences. Lyme disease does not usually cause demyelinating lesions in the cervical or thoracic spine. However, the boundaries between the two diseases are easily blurred, and one disease is often mistaken for the other.
Multiple sclerosis symptoms
Symptoms vary in severity and in prevalence from person to person. Some may experience only a few of those listed below, while others may suffer from a wider range of symptoms. Each flare up of symptoms may bring about new symptoms and the duration might also vary.
Common early signs of MS include fatigue, brain fog, depression, anxiety, poor digestion, vision impairment (blindness, double vision), tingling, numbness, weakness in legs or arms, pain, dizziness, muscle spasms, poor balance and bladder issues.
The following symptoms are also common:
- Optic neuritis — inflammation of the optic nerve. Felt as a sudden onset of visual blurring or loss of vision in one eye, particularly in the central visual field. Eye movement may bring on pain, light flashes, or other visual symptoms.
- Depression — mood disorder with persistent feelings of sadness and loss of interest. Some research suggests that the depression may be caused by the toxins or inflammation that the chronic infections produce.
- Mood swings — from mild to diagnosed Bipolar Affective Disorder, which is more prevalent in the MS community than the general population.
- Balance — vertigo and/or dizziness problems are common in those living with MS, caused by lesions in the areas that coordinate visual, spatial and other input needed to produce and maintain equilibrium.
- Spasticity — can be both intermittent (spasms) and tonic (stiffness) and due to the uncontrollable nature, can add to fatigue, challenges in walking, sitting, and can interfere with hygiene and nursing care in individuals with advanced MS.
- Tremor — an involuntary movement condition. It includes intention tremor, or tremor triggered by voluntary movement, affecting any muscle group including arms, legs, trunk, head, vocal cords, jaws, lips, and tongue.
- Sensory impairment/numbness — an abnormal or lack of sensation, often in one or more limbs. Can gradually spread inward toward the trunk, increasing in extent and intensity.
- Bladder problems — dysfunction in bladder control whether it is a spastic bladder, frequent urinary tract infections or the inability to empty the bladder.
- Chronic pain — can present in many forms and with varying intensity. At least 50% of MS patients report chronic pain as a symptom.
- Sexual dysfunction — both sexual feelings and functions can be affected.
- Heat sensitivity — MS symptoms can become stronger as body temperature increases due to sunbathing, exercise, hot baths, emotion, fatigue, fever, or any increases to the body’s core temperature.
- Difficulty in speaking — otherwise called Dysarthria and can range from mild difficulty annunciating words to speech sounding slurred, garbled, and unclear.
Other symptoms can present relating to any of the above mentioned, including dry mouth, bowel issues, lack of coordination, muscle weakness, chronic fatigue, difficulty in walking, and a range of symptoms related to cognitive impairment.
Early intervention is critical, and it is especially important to pay attention to early warning signs. If any of the above symptoms are presenting without a clear cause or association with another condition, it’s important to address them immediately – the earlier the better to result in a quicker recovery.
What brings on an MS episode?
People with an MS diagnosis may go many years between symptoms, or they may have a long-lasting bout that leads to a gradual or rapid decline in health.
Research is showing with increasing clarity that multiple sclerosis is caused by an infestation of parasites, fungus and bacterial infections in the body, which in turn causes significant inflammation and immune dysfunction.
When the immune system is compromised, environmental factors play a major part in triggering an MS attack, and over time it becomes more difficult to recover and control the disease.
Therefore, it is vitally important to control the external environment as much as possible and watch for the following factors:
High Stress. To keep stress under control, it’s important to understand when stressful situations may arise at work and at home. Learning tools to offset stress (meditation and prayer, time spent in nature, gentle exercise, socializing, hobbies, a routine, counselling or therapy) will prevent stress from further weakening the immune system. Stress management is imperative.
Sleep deprivation. Getting at least 8 hours of quality sleep each night can be achieved by committing to a nighttime routine and using sleep aids if necessary. Also take periodic rests throughout the day if when needed. Investing in optimal sleep can drastically improve immune function.
Other infections. Bouts of MS symptoms can be triggered by a weakened immune system due to other infections such as the flu or UTIs. Along with following the Live Disease eating plan and supporting the body, it is best to avoid situations that may lead to a secondary illness or infection.
Frequent use of antibiotics. Though necessary in certain cases, antibiotics can be overprescribed and can be harmful to a healthy balance of bacteria in the intestinal tract, having dire consequences for those living with multiple sclerosis.
Environmental toxins. Limit exposure to cancer-causing chemicals and endocrine disruptors that includes lead, mercury, radon, formaldehyde, benzene, and cadmium. Human-made chemicals such as BPA, phthalates, and pesticides also belong in this category. Products containing these substances include some plastic bottles and containers, food can liners, detergents, flame retardants, toys, and some cosmetics. To avoid, read labels and research products ahead of time. EMF and RF radiation will cause the chronic infections to grow more quickly and produce more poisons
Mold. Black mold in the home or working environment can hide behind walls, and is prevalent in moist, humid environments. Home testing kits can be purchased, and mold should be immediately eradicated as the mycotoxins greatly suppress immune function.
Food. Food that causes inflammation is detrimental to those trying to keep MS symptoms at bay. Avoid sugar and other sweeteners, refined carbohydrates, gluten, grain, dairy, and avoid processed carbs, caffeine or alcohol. The Live Disease Free eating plan is a low-carb, highly nutritious eating plan that will greatly reduce the food to the infections that are causing the symptoms, resulting in a decrease in inflammation and symptoms.
Each of these external conditions must be controlled in order to support immune function. A weak immune system will allow the underlying infections to be more active, which can result in triggering an MS attack.
Multiple sclerosis by the numbers
Studies show that there has been a steady rise of diagnosed multiple sclerosis cases. In the United States, cases are now around one million people, nearly double reported from prior studies.
The following information is taken from StatsCan, where it is reported that “the prevalence of MS in Canada is among the highest reported in the world. An estimated 93,500 Canadians in private households, and 3,800 in long-term care facilities, have MS.”
MS is most frequently diagnosed between the ages of 20 and 49, with the average age at which people first experience symptoms is 32; a diagnosis may take some time, with the average diagnosis occurring about five years later at age 37.
Life expectancy is shorter for people with MS, with the most common cause of death being MS itself or related complications from the infections. In 2013, of the total 252,338 deaths that occurred in Canada, MS was the underlying cause for 521 (1.5 per 100,000 population).
Women are two to three times more likely than men to have MS. The imbalance in the sex ratio is thought to be increasing in several countries, including Canada — currently the averages are 418 cases per 100,000 women and 159 cases per 100,000 men.
StatsCan also confirms that it is difficult to generalize about the impact of MS because it can manifest in many ways and affect different parts of the body to varying degrees. Statistics they have gathered include:
- Although 57% of people with MS can walk without aid, almost a third (31%) required a wheelchair, a mechanical aid such as a cane or walker, or the help of another person; 12% could not walk at all.
- Just over half (53%) of people living with MS are usually pain-free, with the rest reporting pain that prevented a few activities (21%) or some/most activities (25%).
- Nearly two-thirds (62%) of people experience difficulty getting a good night’s sleep.
The prevalence of MS in Canadian women, especially those who live in colder climates, is increasing. According to a report released in 2006, among people born in the 1930s, about two women contracted MS for every one man, at a ratio of 1.9 to 1. For those born in the 1980s, the incidence has grown to exceed 3.2 cases for every one case among men.
Cases are also more common the further away from the equator. However, climate and cold are not likely common factors since the disease is nearly absent among Canada’s Inuit in the High Arctic and among Indigenous people in North America and Australia; it is also rarely found in Japan.
This is further evidence that the disease is caused by a collection of chronic infections.
Hope for living with multiple sclerosis
Reading through much of the literature online, one might come to feel hopeless, as it is stated again and again that there is no known cause and there is no cure for multiple sclerosis. That the only path forward is symptom management through drugs that might slow the progression of symptoms over time.
However, there is more than 30 years of scientific research in peer-reviewed publications that show what causes MS, allowing a pathway to recovery from it.
Parasites, fungal overgrowth and bacterial infections are always present in people who live with MS, usually at very high levels.
When these infections are treated effectively, through protocols that include diet, lifestyle changes and treating the infections effectively, the disease goes into remission. A person who thought they were to be sentenced to a slow and debilitating condition, who had been living with that condition and the fear that comes along with it, can now find life-changing symptom improvement and even recovery.
In many cases, people experience complete recovery, especially when treated in the early stages of disease. Watching for early signs of symptom development is critical. Again, these include fatigue, brain fog, depression, anxiety, poor digestion, vision impairment (blindness, double vision), tingling, numbness, weakness in legs or arms, pain, dizziness, muscle spasms, poor balance and bladder issues.
An ever growing body of research shows that multiple sclerosis is caused by chronic silent infections in the body. Since this research has not been widely publicized, these factors are often overlooked, leaving people with debilitating symptoms that greatly affect their quality of life.
Treating the infections that cause multiple sclerosis can take months not years but it does require patience and discipline, especially if it is in advanced stages. But it is possible and more and more people are making a full recovery from MS.
It bears repeating: when infections, the root cause of chronic disease are treated effectively, it is possible to recover from MS.

Clinically diagnosed with multiple sclerosis at the age of 28, Pam chose an alternative approach to recovery. Now decades later and still symptom free, she coaches others on how to treat the root cause of chronic disease, using a holistic approach. She can teach you how, too.
Pam is the author of Become a Wellness Champion and founder of Live Disease Free. She is a wellness expert, coach and speaker.
The Live Disease Free Academy has helped hundreds of Wellness Champions in over 15 countries take charge of their health and experience profound improvements in their life.

