Many people diagnosed with MS, and the integrative practitioners treating them, believe the bacteria that causes Lyme disease may actually cause multiple sclerosis. The evidence is substantial: historical research from 1911 onward documented the Lyme bacteria in MS patients, modern pathology finds the same bacteria in MS brain tissue, and clinical studies show 85-90% of MS patients test positive for Lyme disease. The bacteria causes identical symptoms, identical pathology, and an identical disease course. Yet, MS experts aren’t discussing this connection, researching it, or acknowledging it.
The Contradiction
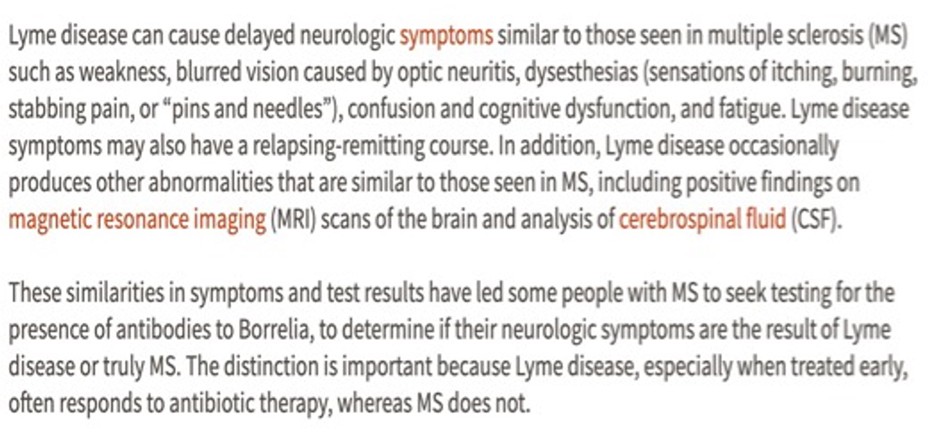
The Multiple Sclerosis Society used to have a page on their website comparing Lyme disease and MS. They acknowledged these conditions often look virtually identical— the same symptoms, the same MRI findings, the same spinal fluid abnormalities, and the same relapsing-remitting course.
The only difference, they claimed: antibiotics work for Lyme, but not for MS.
That webpage is no longer available.
Here is a screenshot of the webpage that was removed:
Interestingly, in 2017, the MS Society of Canada funded research published in the New England Journal of Medicine showing that the antibiotic minocycline significantly reduced MS development in early-stage patients.
So an antibiotic prevented MS in a significant number of people, according to their own study.
So which is it?
A Century of Forgotten Evidence
This contradiction isn’t new. Researchers have documented spirochete bacteria (like the one that causes Lyme disease) in the central nervous system of those with MS since 1911.
The timeline:
- 1911-1922: Multiple studies found spirochete bacteria in MS patients’ cerebrospinal fluid and brain tissue. Published in The Lancet and other major journals.
- 1922: Researchers infected animals with spirochetes from MS patients—the animals developed MS-like symptoms.
- 1950s: Researcher Steiner found spirochetes inside MS brain lesions—at the exact site of damage.
- 1957: Dr. Rose Ichelson cultured spirochetes from MS patients. Her results, published in Time Magazine: 78% of MS patients grew spirochetes. 0% of healthy controls did. She believed spirochetes caused MS and that early treatment could lead to a cure.
Then the research virtually stopped, and by the 1960s, the autoimmune theory took hold and investigation into infections largely ceased.
Why Spirochetes Matter: The Syphilis Proof
In science, it is known that spirochete bacteria cause demyelination.
Neurosyphilis—caused by spirochete bacteria in the central nervous system—produces identical symptoms to MS:
- Demyelination in brain and spinal cord
- Lesions throughout the CNS
- White matter changes on MRI
- Progressive neurological decline.
The symptoms are indistinguishable from MS: muscle weakness, spasticity, cognitive problems, vision issues, tremors, numbness, walking problems, paralysis.
Even spinal fluid shows the same abnormalities: elevated protein, increased white blood cells, oligoclonal bands.
The bacteria that cause syphilis and Lyme disease are both spirochetes—from the same bacterial family.
If one spirochete causes demyelination, and both spirochetes are from the same bacterial family, it’s scientifically reasonable that Borrelia (the bacteria that causes Lyme disease) could cause demyelination too.
Modern Discoveries: Dr. Alan MacDonald
While mainstream medicine embraced the autoimmune theory, pathologist Dr. Alan MacDonald kept investigating.
Using fluorescent antibody staining, he found Borrelia embedded inside myelin sheaths of Alzheimer’s patients—the exact location where MS damage occurs.
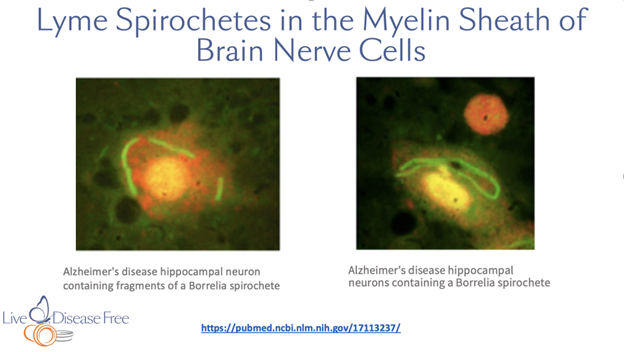
This reframes everything. If bacteria are inside the myelin, the immune system should attack. That’s not autoimmunity—that’s an appropriate immune response with collateral damage.
2016: He examined 10 MS patients and found small parasitic roundworms in 100% of them. When he stained these worms for Borrelia, they lit up—packed with this bacteria.
The mechanism became clear:
- Parasitic worms infected with Borrelia enter the bloodstream
- Worms cross the blood-brain barrier into the CNS
- Worms die, releasing Borrelia
- Bacteria colonize myelin sheaths
- Immune response causes inflammation and demyelination.
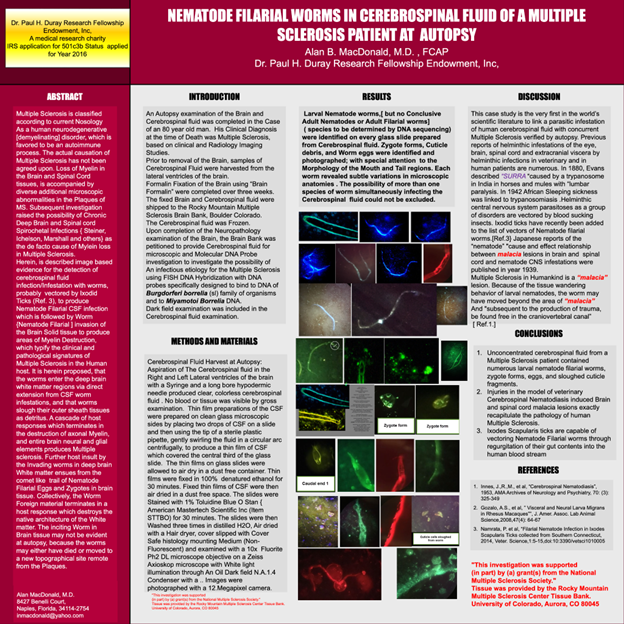
The Worms Act as Trojan Horses
Notably, veterinarians have known for 100+ years that when these worms infect animals’ central nervous systems, they develop MS-like symptoms. These parasites can pass from animals to humans.
2020: Dr. MacDonald found tapeworm larvae and developing juvenile tapeworms in MS patients’ CSF.
Finding tapeworm larvae, developing tapeworms, small roundworms and Borrelia in the CNS revealed that multiple parasites are involved—explaining why MS varies so much between patients.

What Clinicians Are Finding
Dr. Dietrich Klinghardt (Lyme specialist) stated: “We never had…in the last five years a single MS patient…who did not test positive for Borrelia burgdorferi. Not a single one.”
Dr. Richard Horowitz (treated 12,000+ Lyme patients): Calls Lyme “the great imitator” because it mimics MS and other neurological diseases so closely.
Both doctors have successfully treated thousands—including many initially diagnosed with MS—by targeting Borrelia.
Modern Clinical Evidence: The Turkish Study
In a 2019 study from Turkey, researchers tested 126 MS patients for Borrelia burgdorferi.
The results were striking:
108 patients (85.72%) tested positive for Borrelia
Only 18 patients (14.28%) tested negative
This corroborates Dr. Klinghardt’s findings and demonstrates that the Borrelia-MS connection isn’t limited to one country or one clinic—it’s a global pattern.
Why Standard Tests Miss It
If most MS patients have Borrelia, why don’t tests show this?
- Standard ELISA tests miss about 50% of chronic Lyme cases
- Tests target specific strains; other strains go undetected
- Chronic CNS infections may not show circulating antibodies in blood
- Immune suppression reduces antibody production
- Bacteria sequestered in brain tissue don’t appear in blood samples.
Lyme-literate physicians use specialty labs (IGeneX), Western Blot testing, clinical diagnosis, energy testing and others. With sensitive approaches, most MS patients test positive.
The Norwegian Lyme Cyst Study (Explains Detection Problems)
In a study by Norwegian scientists, researchers examined 10 MS patients and found cyst forms of Borrelia spirochete bacteria in all 10.
No bacteria were found in control subjects.
Critically, when these cysts were cultured, they transformed into spirochetal bacteria.
This explains why detection is so difficult: Borrelia exists in multiple forms:
- Active spirochetes (standard form)
- Cystic L-forms (dormant, difficult to detect)
- Biofilm communities
The bacteria can shift between forms to evade the immune system and antibiotics. Standard tests look for active spirochetes and miss the cystic forms entirely.
Recent Official Recognition of Lyme Disease by WHO
On June 18, 2018, the World Health Organization issued the 11th revision of the International Classification of Diseases (ICD-11), officially recognizing for the first time in over 25 years:
- 1C1G.2 Congenital Lyme borreliosis
- 6D85.Y Dementia due to Lyme Disease
- 8A45.0Y Central nervous system demyelination due to Lyme borreliosis
“Central nervous system demyelination due to Lyme borreliosis.”
The WHO is now officially recognizing that Lyme disease causes CNS demyelination—the defining pathology of MS.
The European Parliament Lyme Disease Resolution (2018)
On November 15, 2018, the European Parliament adopted its first-ever resolution on Lyme disease, calling on the European Commission to:
- Draw up a plan to combat Lyme disease
- Implement mandatory reporting in all Member States
- Promote better exchange of best practices
- Provide additional funding for diagnostic and treatment methods
- Support research efforts
The growing institutional recognition that Lyme is a serious, widespread problem makes the MS-Lyme connection increasingly difficult to dismiss.
The Evidence Summary
Historical: 100+ years of peer-reviewed research documenting spirochetes in MS patients
Biological: Neurosyphilis proves spirochetes cause CNS demyelination
Pathological: Borrelia found in myelin sheaths; parasitic worms carry Borrelia found in 100% of MS patients tested
Clinical: 90%+ of MS patients test positive for Borrelia with proper testing; symptoms often indistinguishable from Lyme
Treatment: MS Society-funded research shows antibiotics prevent MS development in early MS; historical and modern reports of improvement with antimicrobial treatment
Same symptoms. Same test results. Same MRI findings. Same organism. Same antibiotic response.
When will the experts acknowledge Borrelia may cause MS?
Treatment Implications
If MS is caused by infection, then MS is treatable.
I know this from experience. Thirty-five years ago at age 28, I was diagnosed with MS and told it was incurable autoimmune disease.
I treated parasites and I’ve been MS free for over 35 years.
I’ve since worked with thousands of student using this approach helping them to treat the root cause and recover.
This wouldn’t be possible if MS were truly autoimmune.
The Questions That Demand Answers
The evidence has existed for over 100 years. It’s documented, reproducible and published in prestigious journals.
Why do we still call MS incurable and autoimmune?
Why aren’t neurologists testing for Borrelia?
Why aren’t we treating the infection documented since 1911?
While paradigms are protected, people suffer terribly and die prematurely.
And evidence suggesting treatment has existed since 1957.
There are real solutions to recover from parasites today!
To restore health, we must focus on treating the cause of inflammation, which are parasites. First, identify the enemy (parasites), then support the body and treat the parasites while following a holistic approach. When parasitic infections are treated effectively, we can overcome inflammation or disease.
If you’re frustrated with the fact that our standard of care STILL doesn’t offer a real solution for treating MS and other diseases, then click on the link below to watch Pam Bartha’s free masterclass training and discover REAL solutions that have allowed Pam and many others to live free from MS and other diseases.
CLICK Here to watch Pam’s masterclass training
References:
References at LiveDiseaseFree.com.
https://livediseasefree.com/ms-infections-not-chron/
MacDonald AB. Alzheimer’s disease Braak stage progressions: reexamined and redefined as Borrelia infection transmission through neural circuits. Med Hypotheses. 2007;68(5):1059-1064.
https://pubmed.ncbi.nlm.nih.gov/17113237/
MacDonald AB. Alzheimer’s and Borrelia. 2016. Video.
https://www.youtube.com/watch?v=EHVXJpDBcmU
Metz LM, Li D, Traboulsee AL, et al. Trial of Minocycline in a Clinically Isolated Syndrome of Multiple Sclerosis. N Engl J Med. 2017;376(22):2122-2133.
https://pubmed.ncbi.nlm.nih.gov/28564557/
Under Our Skin full documentary. YouTube.
https://www.youtube.com/watch?v=YMQC4xoAWhg
Horowitz RI. Why Can’t I Get Better? Solving the Mystery of Lyme and Chronic Disease. New York, NY: St. Martin’s Press; 2013.
Klinghardt D. “Under Our Skin” [Documentary film]. Open Eye Pictures; 2008. https://www.youtube.com/watch?v=YMQC4xoAWhg
Schaller JL, Burkland GA. Novel brain compartment tapeworm larvae in multiple sclerosis: 10 patients [PDF]. ECMI. 2021. https://www.ilads.org/wp-content/uploads/2021/05/ECMI-17-01109-Novel-brain-Compartment-Tapeworm-Larvae-in-Multiple-Sclerosis-10-patients-PDF.pdf
Dr MacDonald. Nematode filarial worms in cerebral spinal fluid of a multiple sclerosis patient at autopsy. 2016 https://f1000research.com/posters/5-79
MacDonald. Multiple sclerosis autopsy cerebrospinal lateral ventricle fluids demonstrate coenurus parasites- 10 patients – 1984-2014. Poster: F1000Research. 2021. Poster No. 9-1062.
https://f1000research.com/posters/9-1062
Horowitz RI, Freeman PR. Efficacy of double-dose dapsone combination therapy in the treatment of chronic Lyme disease/post-treatment Lyme disease syndrome (PTLDS) and associated co-infections: a retrospective chart review. Antibiotics (Basel). 2020;9(11):725.
https://pmc.ncbi.nlm.nih.gov/articles/PMC7690415/
Barbaros Çeti. Frequency of Borrelia burgdorferi Western Blot and LTT positivity among multiple sclerosis patients from Turkey. Parasitic worms and multiple sclerosis. EJBPS, 2019, Volume 6, Issue 4, 27-32 https://journals.indexcopernicus.com/api/file/viewByFileId/749551

Clinically diagnosed with multiple sclerosis at the age of 28, Pam chose an alternative approach to recovery. Now decades later and still symptom free, she coaches others on how to treat the root cause of chronic disease, using a holistic approach. She can teach you how, too.
Pam is the author of Become a Wellness Champion and founder of Live Disease Free. She is a wellness expert, coach and speaker.
The Live Disease Free Academy has helped hundreds of Wellness Champions in over 15 countries take charge of their health and experience profound improvements in their life.

