There are insightful connections between the distribution of MS and malaria in many countries. It is also fascinating how MS patients have experienced symptom improvements when prescribed malaria drugs. This post discusses this forgotten research and how it may help in the treatment of MS.
In Part 1 of this series, I reviewed a 2021 study from the University of Calgary, Alberta, Canada which found that Primary Progressive MS patients who received hydroxychloroquine for 1.5 years experienced a significant reduction in the progression of disability. Review part 1 here.
In Part 2 of this series, I reviewed the findings of the research review, Is multiple sclerosis caused by a silent infection with malarial parasites? A historico-epidemiological approach: part I.
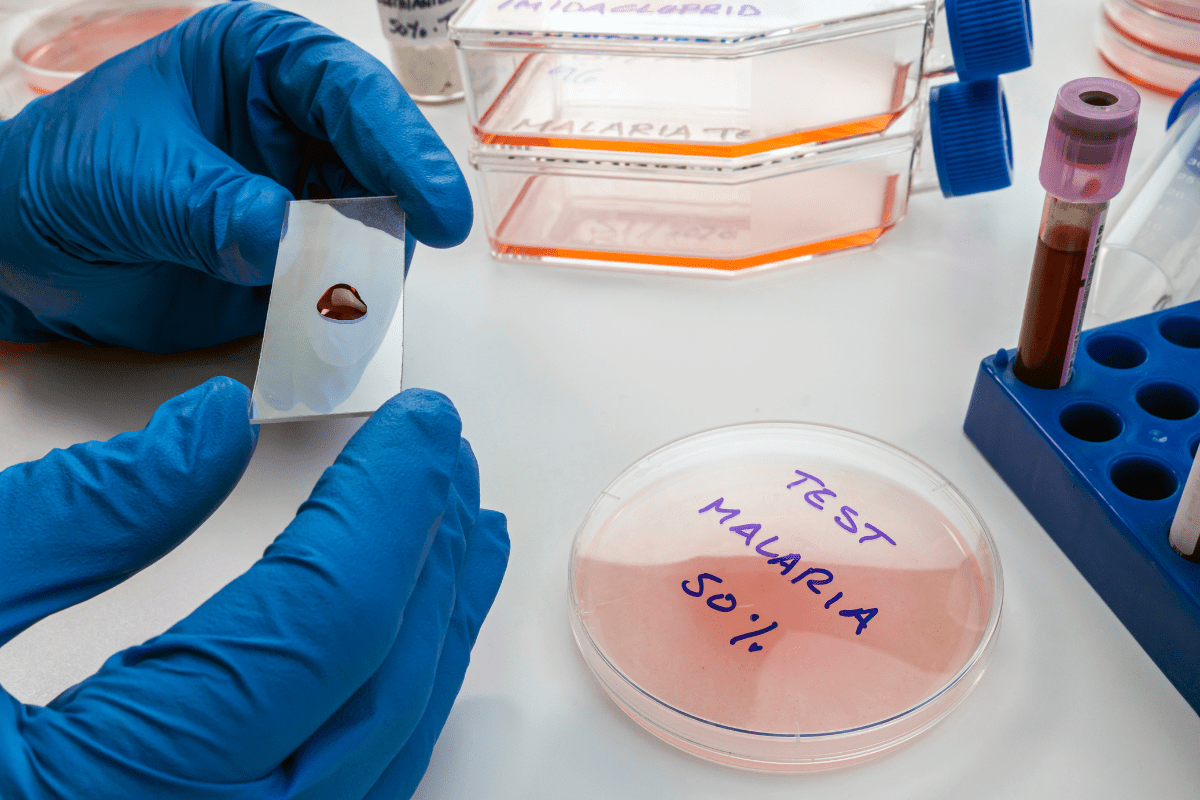
The author shared research about the discovery of antibodies and malaria parasites in multiple sclerosis (MS) patients.
By examining the distribution of MS and malaria and the presence of malaria antibodies and parasites in MS patients, he concluded that an infection with malarial parasites in early childhood could prevent the later development of MS, while a silent infection of malaria during adolescence or adulthood in people not immune to malaria, could likely be the cause of MS. Review part 2 here.
This post is part 3 and the final part of this series. Here, we review the second research review by Kissler, Is multiple sclerosis caused by a silent infection with malarial parasites? A historico- epidemiological approach: part II.
[Note] The following research in this post highlights the research Kissler showcased in part II of his study and his conclusions about the findings of the research.
From the results of various studies, Kissler believed that the global distribution of MS could be the result of “the steadily declining immunity against the different species of plasmodia [the parasite that causes malaria], which started in the middle of the 19th century first in the mountainous areas of northern Europe, to approximately the end of the 19th century in northern America and gradually spreading to the south.”[i]
It is important to note that the transmission of malaria does not stop when clinical epidemics of malaria disappears, but instead it becomes a silent chronic infection and the distribution of malaria keeps to its former pattern over a longer period of time.
The author discusses the distribution of malaria in countries like Sweden, Finland, Italy, Switzerland and others.
In certain climates where malaria was epidemic, MS rates were low at the time of the epidemic.
At higher elevations (within the same countries where malaria was epidemic and thus not farther from the equator), malaria was not epidemic but a chronic silent infection. Temperatures in the summer must be at least 15 degrees Celsius in the temperate zone for malaria to spread. In cities and towns with higher elevations, because there were less malaria parasites infecting mosquitoes, people had less immunity to malaria and would be more susceptible to a more chronic form of malaria.
Several researchers compared the distribution maps of MS and malaria and found meaningful connections.
Switzerland
Switzerland has the most extensive statistics on the distribution of multiple sclerosis. Two different research groups showed that most cases of MS were in the northern part of Switzerland.
Malaria had been endemic mainly in the southern part of Switzerland where they had significantly fewer cases of MS.
Scientists believe that the areas with high malaria infection did not completely disappear from Switzerland when many infected people were treated, malaria changed from an active visible or acute form of infection to a chronic silent infection form of malaria.
In 1970, researchers Wüthrich and Rieder published a paper about seasonal incidences of MS flares in various parts of Switzerland. They found that the maximum incidences of MS attacks were in spring and the minimum in autumn, with a significant difference between the two seasons.
This observation was in agreement with the findings of researcher Neergard who found a seasonal incidence of malaria , that had been observed between 1916 and 1920 in Klosters, Switzerland.
The prevalence of MS in relation to altitude
Malaria could not be found in Germany above an altitude of 400 to 500 m, or in Italy between 600 to 1000 m.
The higher the altitude, the less the transmission of malaria. Therefore, if malaria causes MS, altitude and latitude are both important factors.
Kissler shows good evidence of a positive link between the prevalence of MS and altitude. Surveys in Germany, Norway, Czechoslovakia and Italy have all shown that altitude impacts the incidence of MS. The prevalence of MS was significantly higher in regions with a lower mean temperature and a greater altitude. This suggests that at higher altitudes the prevalence of MS is higher.
Someone born and raised in a town in Sicily which was located at a high altitude, had very little chance of acquiring an immunity against malaria in their childhood.
When, later as an adolescent or adult, if they left the mountainous area of Sicily, and moved to an area where there wasn’t an epidemic of malaria but instead a high silent malaria transmission rate compared to their home town in the coastal area of Sicily, they ran the risk of contracting chronic malaria or MS.
Also researchers have shown that if summers are hot, malaria can occasionally be transmitted in higher regions of Sicily.
Silent Epidemics of Malaria
In the study of malaria, lightly infected insects can cause failed or even dormant cases of malaria. A low-grade malaria infection in a human, even when immature forms of malaria are not found in blood work, can still be transmitted from humans back to mosquitoes.
With a high prevalence of MS in mountainous regions, Kissler felt that the logical conclusion would be that a real epidemic of malaria should later be followed by an increase of cases of MS.
Mississippi
Floods caused by the Mississippi river occurred in 1903, in 1912 and again in 1913.
It is a well-known fact that floods in an area where malaria is already endemic are followed by an increase of mosquitoes because of the better breeding opportunities and thus an increase in malaria follows extensive flooding.
These floods in Mississippi did result in a much higher incidence of malaria.
Mississippi showed by far the highest percentage of positive cases of malaria at 31.1%, while the average of all states (Mississippi included) was 13.28%.
The author thought that this could explain the high rate of cases of MS among the ‘drafted men’ from the state of Mississippi in 1917 which followed the epidemic of malaria.
Treating MS with Quinine
Historically, there have been many cases of patients with MS symptoms, who were thought to have malaria and were cured with the malarial drug quinine.
In 1917, Castellani wrote: “I have seen one case in the Balkans, and three in the Tropics, of a malarial condition closely simulating disseminated sclerosis, with scanning speech, intentional tremor, nystagmus, spastic gait, and increased reflexes. All the cases were cured by quinine.”[i]
He concluded that just because these cases responded well to the treatment with quinine, they could not have been real, genuine MS.
Many years ago, Muller, Marburg and Brickner all felt that quinine was helpful in the treatment of MS.
Brickner in New York treated about 50 MS patients over 5 years between 1930 and 1935.
His conclusion – “The experience of five years with forty-nine patients seems to justify the conclusion that quinine is beneficial in cases of multiple sclerosis, particularly in the early stages’.” He once again stated, “A general view of the present status of the forty-nine patients as individuals strongly indicates that quinine therapy has been helpful.”[i]
Herxheimer reaction
Brickner found that in some cases of treating MS with quinine, there was a slight increase in symptoms followed by marked improvement. He believed that the initial downturn in health was a good sign that the drug would be helpful.
The term Herxheimer reaction was first discussed in the early stages of treating syphilis, which is a bacteria similar to Borrelia, the bacteria that causes Lyme disease.
When quinine was given at a low dose, it had the ability to produce an attack (often a fever) of malaria in people who suffered with a chronic form of malaria.
Craigs Conclusion
In 1917, Craig, without having seen a single parasite, concluded from the feverish reaction that he observed in a patient with MS after the administration of quinine, that the patient most likely had malaria.
He wrote that “the enlarged spleen, the history of typical malarial attacks and the characteristic reaction of chronic malaria to quinine were sufficient evidence, without the presence of plasmodia, to attribute lesions in the patient’s central nervous system to malarial infections.”[i]
In 1921, Mühlens stated that the injection of small doses of quinine had become a well-known method to detect malaria as it showed parasites for the first time after the administration of quinine.
Similarly in 1945, Perret-Gentil in Switzerland, re-examined the value of this controversial method of diagnosing uncured malarial infections, commented that it is advisable to look for parasites at the moment when a treatment with quinine is started. It was then that he was able to observe bouts of fever together with the parasites.
There is over 100 years of research linking multiple sclerosis to the parasite that causes malaria. The distribution of malaria and MS, the presence of malaria antibodies and malaria parasites in MS patients, the seasonality of MS and malaria, and the the fact that several researchers who treated MS patients with quinine found significant improvements in their patients, all indicate that malaria probably plays a role in multiple sclerosis.
All this very important research has been forgotten until 2021 when the University of Calgary, Alberta, Canada published their study showing that primary progressive MS patients given hydroxychloroquine for about a year and a half experienced a significant decrease in the progression of disability.
From our experience in supporting over 1000 students in their recovery from MS, I don’t believe that the malaria parasite is the only cause of MS but it may be a significant parasite in many MS patients. This research must explored further.
There are Real Solutions for MS Today!
To restore health, we must focus on treating the cause of inflammation, which are parasites. First, identify the enemy (parasites), then support the body and treat the parasites while following a holistic approach. When parasitic infections are treated effectively, we can overcome inflammation or disease.
If you’re frustrated with the fact that our standard of care STILL doesn’t offer a real solution for treating MS, then click on the link below to watch Pam Bartha’s free masterclass training and discover REAL solutions that have allow Pam and many others to live free from MS symptoms.
CLICK Here to watch Pam’s masterclass training
Or take the Health Blocker Quiz to see if you could have parasite infections
References:

Clinically diagnosed with multiple sclerosis at the age of 28, Pam chose an alternative approach to recovery. Now decades later and still symptom free, she coaches others on how to treat the root cause of chronic disease, using a holistic approach. She can teach you how, too.
Pam is the author of Become a Wellness Champion and founder of Live Disease Free. She is a wellness expert, coach and speaker.
The Live Disease Free Academy has helped hundreds of Wellness Champions in over 15 countries take charge of their health and experience profound improvements in their life.

